Thank you to Margaret Kidd, library archivist at the VCU Tompkins-McCaw Library for the Health Sciences, for organizing another stellar visit earlier this month to the Special Collections and Archives. Images are below.
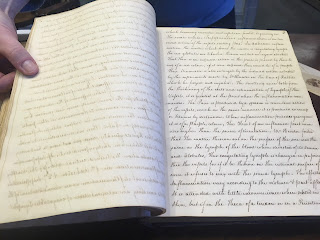
In the assortment of rare books and manuscripts viewed on the day, my favorite was John Huxham's Essay on Fevers, an 18th century treatise on infectious diseases (prior the the germ theory of infection).
Why do I frequent the medical library, particularly in this digital age?
To be inspired and to be given a figurative kick in the academic pants so as to keep researching and publishing. Also, I just like books and cool open spaces. There are worse pastimes.
This is my last blog posting of 2017. Thank you to the few who regularly follow my blog.
Happy New Year.
 |
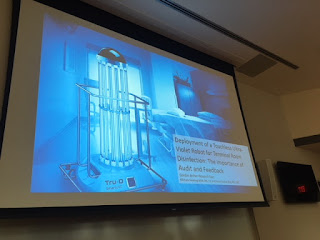
| Medical College of Virginia, 1844 |
 |
| Medical Archives Collection |
 |
| John Huxham's Essay on Fevers- 1755 |